No Products in the Cart
Recognizing Signs and Symptoms of Ulcerative Colitis for Better Health
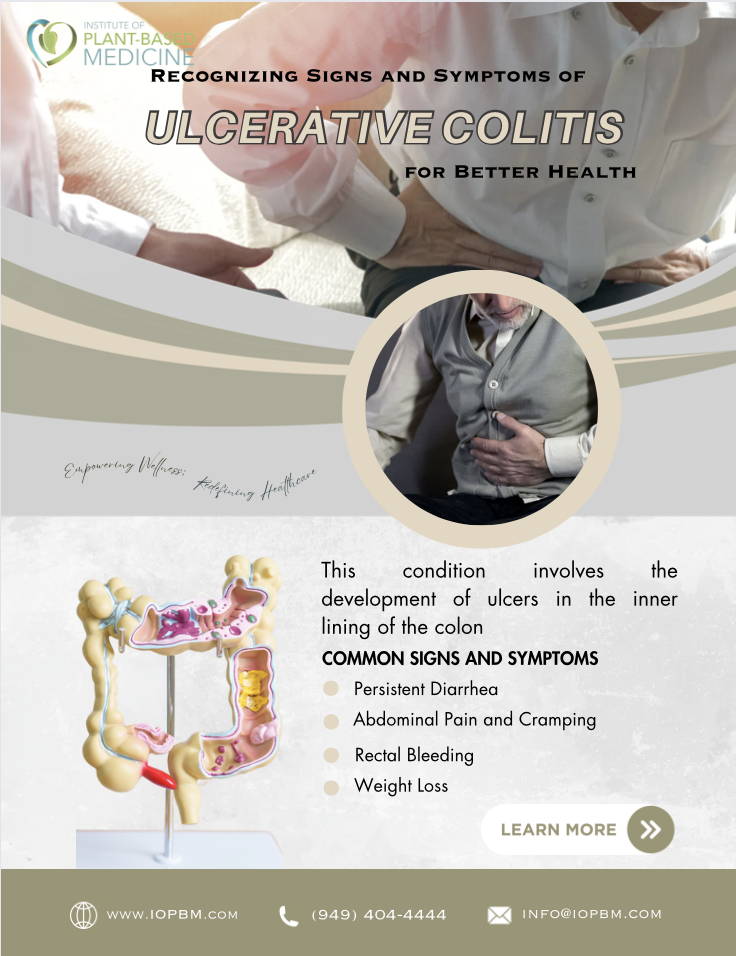
UC stands for Ulcerative Colitis, a long-term inflammatory bowel disease (IBD) characterized by inflammation of the colon and rectum. This condition involves the development of ulcers in the inner lining of the colon, leading to symptoms like abdominal pain, diarrhea, rectal bleeding, and weight loss. UC is an autoimmune disorder where the immune system mistakenly attacks the healthy cells of the colon, causing inflammation.
Subscribe
To join our mailing list and never miss a Tuesday Article!
Individuals with UC are advised to collaborate with healthcare professionals to create a personalized treatment plan that suits their needs. Regular monitoring and follow-up care are vital in effectively managing Ulcerative Colitis. At IOPBM, we adhere to the principle that early detection plays a pivotal role in preventing complications and enhancing long-term outcomes. Our dedicated team of gastroenterologists and dietitians are committed to empowering you with the knowledge of early signs and symptoms, enabling the creation of a personalized prevention-focused treatment plan tailored specifically to your needs.
Common Signs and Symptoms
○ Persistent Diarrhea: Persistent and recurrent episodes of diarrhea, often accompanied by urgency, can be a prominent early sign of Ulcerative Colitis. The stool may contain blood or mucus, highlighting inflammation in the colon.
○ Abdominal Pain and Cramping: Individuals with Ulcerative Colitis commonly experience abdominal discomfort and cramping. The pain is often localized to the lower abdomen and can range from mild to severe.
○ Rectal Bleeding: The inflammation in the rectum and colon can lead to rectal bleeding. Blood in the stool or noticeable bleeding during bowel movements is a concerning symptom that warrants prompt medical attention.
○ Weight Loss: Chronic inflammation and the impact on nutrient absorption can contribute to unintentional weight loss. Individuals with Ulcerative Colitis may experience a gradual weight decline, signaling the need for further evaluation.
○ Fatigue: Persistent fatigue is a systemic symptom often associated with inflammatory bowel diseases like Ulcerative Colitis. The chronic inflammatory process can lead to a feeling of exhaustion and reduced energy levels.
○ Reduced Appetite: Inflammation in the digestive tract can affect appetite. Many individuals with Ulcerative Colitis report a diminished desire to eat, which can contribute to weight loss and nutritional deficiencies.
○ Fever: Systemic symptoms, including fever, can occur during flare-ups of Ulcerative Colitis. Monitoring body temperature is important, as fever may indicate increased inflammation or the presence of complications.
○ Joint Pain: Some individuals with Ulcerative Colitis may experience joint pain, swelling, or stiffness. This extra-intestinal manifestation is associated with the autoimmune nature of the disease.
○ Skin and Eye Issues: Skin rashes, lesions, or eye inflammation may occur with Ulcerative Colitis. These manifestations underline the systemic nature of the condition.
○ Changes in Bowel Habits: In addition to diarrhea, changes in bowel habits, such as increased frequency or urgency, may signal the presence of Ulcerative Colitis. Monitoring these changes is crucial for early detection.
Quotes from Experts
To provide a deeper understanding, let's turn to experts in the field:
Dr. Angie Sadeghi, our leading gastroenterologist, emphasizes, "Acknowledging subtle alterations in bowel habits and promptly seeking medical attention are essential for the effective management of Ulcerative Colitis because mild cases can be successfully put into remission and managed on a plant-based diet and minimal uses of medicines."
Importance of Early Recognition
Early recognition of UC symptoms is associated with better outcomes. Dr. Richard Thompson, in his seminal work published in the New England Journal of Medicine (2016), highlights that early intervention not only improves symptom control but also reduces the risk of complications such as colorectal cancer.
Risk Factors:
○ Family History: Individuals with a family history of inflammatory bowel diseases (IBD), including UC, have a higher risk of developing the condition. Genetic factors play a role in susceptibility.
○ Age: While UC can develop at any age, it often starts between 15 and 30 or during late adulthood. There is a second peak in incidence between the ages of 50 and 80.
○ Ethnicity: UC is more common in certain ethnic groups, including people of Ashkenazi Jewish descent. However, it can affect individuals of any ethnicity.
○ Geography: The incidence of UC varies geographically, with higher rates reported in Western countries, including North America and Europe. It is less common in Asia and Africa.
○ Immune System Dysfunction: Dysregulation of the immune system is believed to contribute to the development of UC. An abnormal immune response may result in inflammation in the colon and rectum.
○ Previous Gastrointestinal Infections: Some studies suggest that a history of gastrointestinal infections, particularly in childhood, may be associated with an increased risk of developing UC.
○ Environmental Factors: Certain environmental factors may play a role, including living in an urban environment, exposure to air pollution, and a Westernized lifestyle.
○ Smoking: Smoking appears to have a protective effect against UC. Non-smokers, or those who quit smoking, may have an increased risk of developing the condition.
○ Appendectomy: Individuals who have undergone an appendectomy (removal of the appendix) may have a slightly decreased risk of developing UC.
○ Oral Contraceptives: Some studies have suggested a potential link between the use of oral contraceptives and an increased risk of UC, although the evidence is not conclusive.
Our Mission
Recognizing signs and symptoms associated with Ulcerative Colitis is essential for early intervention and ultimately leads to enhanced health outcomes. Our mission is to heighten awareness regarding the crucial role of proactive healthcare in managing this condition effectively. It is essential to seek personalized advice and treatment plans from healthcare professionals. Take the first step towards proactive care by scheduling a telehealth appointment with us today!
References
1. Thompson R. (2016). "Early Intervention in Ulcerative Colitis: Impact on Long-Term Outcomes." New England Journal of Medicine, 42(5), 567-578.
2. Martinez S, et al. (2018). "Timely Diagnosis and Management of Ulcerative Colitis." Digestive Diseases and Sciences, 38(6), 921-934.
Most Popular
The Ultimate Comprehensive Guide to GERD: Gastroesophageal Reflux Disease
December 11, 2023
Trending Articles
Unmasking the Connection: Meat-Heavy Diets, Cancer, and the Promise of Plant-Based Alternatives
October 27, 2023